Eczema, also known as atopic dermatitis, is a common inflammatory skin disorder affecting over 230 million people worldwide. This figure comes from recent global reports shows the impact of atopic dermatitis, especially in regions with rising pollution and changing lifestyles. It’s more than just “dry skin”, this chronic condition can cause intense itching, redness, discomfort, and significantly reduce quality of life during flare-ups.
In this guide, you can explore what eczema is, its key symptoms, possible causes, and effective treatment options available in 2025.
What is Eczema?
Eczema is a chronic skin condition that causes inflammation, dryness, itching, and rashes. It occurs when the skin’s natural barrier is weakened, making it more sensitive to irritants and allergens.
There are different types of eczema, but the most common is atopic dermatitis. It often begins in childhood but can appear at any age. While eczema is not contagious, it can be persistent and flare up at certain times.
Symptoms of Eczema
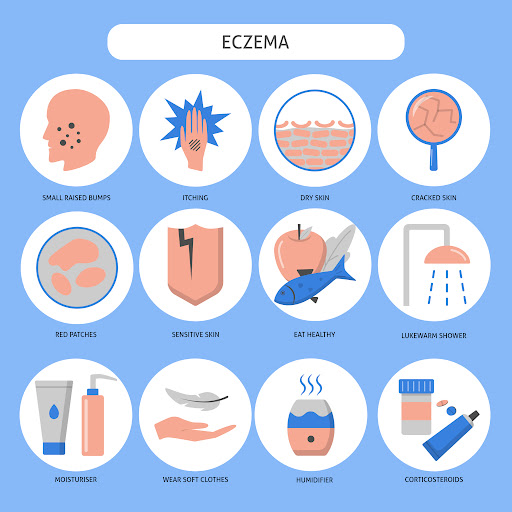
Eczema symptoms vary from person to person, but usually include:
- Dry, itchy skin – often worse at night.
- Red or brownish-gray patches – commonly on the hands, feet, ankles, wrists, neck, eyelids, elbows, and knees.
- Thickened or scaly skin – due to repeated scratching.
- Small, raised bumps – which may leak fluid when scratched.
- Inflamed or swollen skin – during flare-ups.
In children, eczema often appears on the face, scalp, or cheeks, while in adults, it tends to affect the hands and areas behind the knees.
Causes of Eczema
The exact cause of eczema (also known as atopic dermatitis) is still not completely understood, but researchers agree that it develops from a complex interplay of genetics, the immune system, and environmental factors. These elements disrupt the skin’s natural protective barrier, making it more prone to dryness, irritation, and inflammation. Below are the primary contributing factors:
Genetics
Eczema often runs in families. People with a family history of eczema, asthma, or hay fever are at a higher risk of developing the condition. This genetic link suggests that inherited traits affect how the skin barrier functions and how the immune system responds to triggers.
Immune System Dysfunction
In eczema, the immune system tends to overreact to irritants or allergens. Even mild triggers can cause the body to release inflammatory chemicals, leading to redness, itching, and flare-ups. This exaggerated immune response is one reason eczema is considered a chronic inflammatory condition.
Weakened Skin Barrier
A healthy skin barrier locks in moisture and keeps out bacteria, allergens, and irritants. In people with eczema, this barrier is often weaker or compromised, leading to dryness, cracks, and increased sensitivity. As a result, the skin loses moisture more easily and becomes vulnerable to infections.
Environmental Triggers
External factors are some of the most common eczema triggers. Everyday elements such as pollen, dust mites, harsh soaps, detergents, fragrances, and pet dander can irritate sensitive skin. Continuous exposure to these triggers can worsen flare-ups and delay healing.
Weather and Climate
Climate conditions play a significant role in eczema symptoms. Cold, dry air can strip moisture from the skin, while hot and humid weather can increase sweating, which may lead to itching and irritation. Seasonal changes often worsen symptoms for many people.
Stress
Emotional and psychological stress is a well-known eczema trigger. Stress doesn’t directly cause eczema, but it can weaken the immune system and intensify flare-ups, making existing symptoms worse and harder to manage.
ALSO READ
How to Treat Acne Scars – 10 Effective Home Remedies For A Beautiful Skin
Treatment Options for Eczema
Eczema has no permanent cure, but with the right treatment plan, flare-ups can be controlled, and symptoms can be greatly reduced. The goal of treatment is to calm inflammation, restore the skin barrier, and minimize itching so that people can enjoy a better quality of life.
One of the first and most effective steps is daily skincare management. Hydration is critical because eczema-prone skin loses moisture quickly, making it more vulnerable to irritation. Dermatologists recommend applying fragrance-free moisturizers several times a day and using mild cleansers instead of harsh soaps. Taking short, lukewarm showers and moisturizing immediately afterward helps lock in hydration. Avoiding chemical-based detergents and strong perfumes also reduces the risk of flare-ups.
When flare-ups become more severe, medications often play an essential role. Topical corticosteroid creams help reduce inflammation and itching quickly, while non-steroid creams like tacrolimus are used for sensitive skin areas such as the face. For people who experience intense nighttime itching, antihistamines can provide relief and improve sleep. In more serious cases, doctors may prescribe advanced biologic drugs such as dupilumab, which target the immune system directly and provide long-term relief.
For patients who do not respond well to topical treatments, light therapy (phototherapy) can be an effective alternative. This method uses controlled exposure to ultraviolet (UV) light, which helps slow the immune system’s overreaction and reduces inflammation. Many patients experience significant improvements with this therapy, but it must be done under medical supervision to avoid risks like burns or long-term UV damage.
Finally, home remedies and lifestyle changes are just as important as clinical treatments. Natural solutions such as aloe vera, oatmeal baths, and coconut oil provide soothing relief for irritated skin. Wearing breathable fabrics like cotton instead of wool prevents additional irritation, while stress management techniques, like yoga, meditation, and deep breathing. They all can minimize emotional triggers that can worsen symptoms.
To summarize, managing eczema often requires a combination of strategies:
- Skincare and Hydration – Consistently moisturizing and avoiding harsh products keeps the skin barrier strong.
- Medications – Topical steroids, non-steroid creams, antihistamines, or biologics may be prescribed depending on severity.
- Phototherapy – Controlled UV light therapy helps reduce inflammation in moderate to severe cases.
- Lifestyle Adjustments – Stress reduction, natural remedies, and wearing soft fabrics can prevent flare-ups and ease symptoms.
With this holistic approach, eczema can be managed effectively even if it cannot be fully cured. Consistency and personalized care are the keys to keeping flare-ups under control and maintaining healthy skin.
Prevention Tips For Eczema
- Keep your skin well-hydrated daily.
- Identify and avoid personal triggers (like perfumes, allergens, or certain foods).
- Use a humidifier in dry environments.
- Stick to dermatologist-approved skincare routines.
Sum Up
Eczema is a chronic but manageable condition. Understanding its symptoms and triggers is the first step toward relief. With modern treatments, from advanced biologics to simple skincare routines, people with eczema can live comfortably and reduce flare-ups. Consulting a dermatologist ensures you get the right treatment plan tailored to your skin’s needs.
FAQs
Can eczema go away completely?
In some children, eczema symptoms may fade as they grow older, especially if flare-ups are mild. However, for many, eczema continues into adulthood as a chronic condition. The good news is that with proper skincare, medical treatment, and lifestyle changes, flare-ups can be managed effectively, making it easier to live a comfortable life.
What foods trigger eczema?
Food triggers differ from person to person, but common ones include dairy, eggs, nuts, wheat, soy, and shellfish. Some people notice flare-ups after consuming processed or sugary foods as well. Keeping a food diary and consulting with a doctor or allergist can help identify personal triggers.
Is eczema contagious?
No, eczema is not contagious. You cannot “catch” it from someone else since it is caused by a mix of genetics, environment, and immune system responses. However, scratching the skin can sometimes lead to infections, so it’s important to treat flare-ups promptly to avoid complications.
Can stress really cause eczema flare-ups?
Yes, stress is a major trigger for many people with eczema. When you’re stressed, your body releases hormones that increase inflammation, worsening itching and redness. Stress management techniques such as yoga, meditation, journaling, or even light exercise can significantly reduce flare-ups.
What is the best treatment for severe eczema?
Severe eczema often requires prescription treatments, including stronger topical corticosteroids, oral medications, or advanced biologic injections like dupilumab. Dermatologists may also recommend light therapy or combination approaches. Personalized treatment plans ensure that flare-ups are reduced and skin stays healthy in the long term.



Join The Discussion